When you hear about lumbar myelopathy, you might wonder what exactly happens in your spine to cause such discomfort. This condition involves compression or damage to the spinal cord in your lower back, leading to pain, numbness, or weakness in your legs. Understanding its causes and symptoms is essential, but knowing when to seek medical advice can be even more critical. If you’re curious about how it’s diagnosed and the range of treatment options available, there’s more to explore. What proactive steps can you take to manage this condition effectively?
Key Takeaways
- Lumbar myelopathy is a condition caused by compression of the spinal cord in the lumbar spine region.
- Common causes include spinal stenosis, herniated discs, degenerative diseases, and traumatic injuries.
- Symptoms may include back pain, leg weakness, numbness, and changes in bowel or bladder function.
- Diagnosis typically involves imaging tests like X-rays, MRIs, and nerve function assessments such as EMGs.
- Treatment options range from nonsurgical methods like physical therapy to surgical interventions like spinal decompression.
Understanding Lumbar Myelopathy
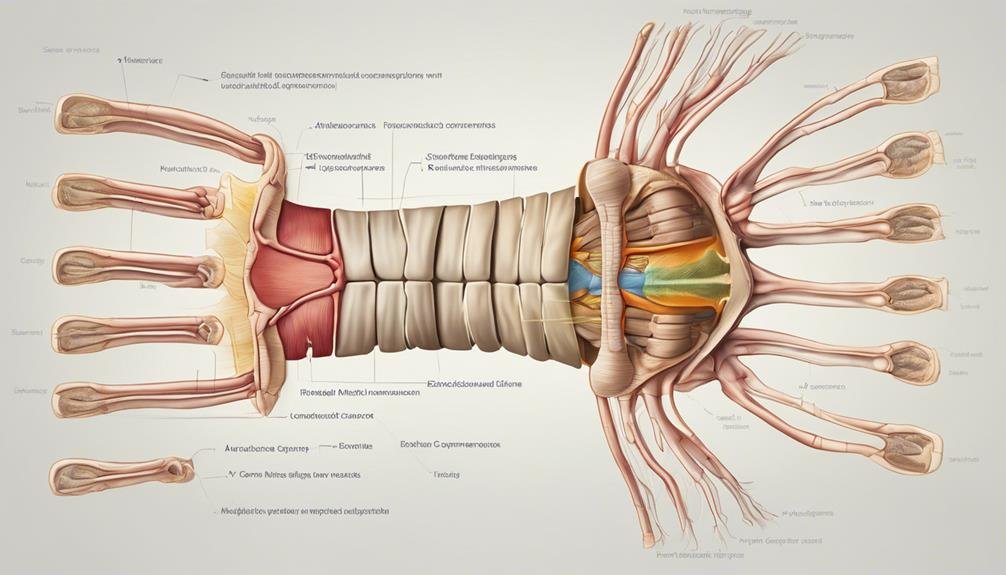
Lumbar myelopathy, often obscure, is a condition caused by spinal cord compression in the lower back region. You may wonder how such compression occurs. It’s often due to factors like herniated discs, spinal stenosis, or even tumors pressing on the spinal cord. This pressure can disrupt the normal function of the spinal nerves, leading to a range of issues.
Understanding lumbar myelopathy is important because early recognition and treatment can prevent further damage. Treatments vary depending on the severity of the compression and the symptoms you’re experiencing. Generally, initial approaches might involve medication to reduce inflammation and physical therapy to strengthen the muscles around the lumbar area. These can help alleviate some pressure on the spinal cord and improve mobility.
In more severe cases, surgical intervention, such as spinal decompression surgery, may be necessary. This procedure aims to relieve the compression on the spinal nerves, providing relief from symptoms and preventing permanent damage.
Proactively seeking treatment can greatly improve your quality of life and reduce the risk of long-term nerve damage associated with lumbar myelopathy.
Symptoms of Lumbar Myelopathy
Recognizing the symptoms of lumbar myelopathy is essential for timely intervention and effective management. You might notice pain in your lower back or legs, which can be an early indication of this condition. Often, numbness and tingling in the lower body accompany this pain, potentially spreading to other areas. Weakness in the legs can make simple tasks like walking more challenging, and you may experience a noticeable loss of balance. Coordination issues could arise, affecting your ability to perform fine motor tasks.
| Symptom | Impact |
|---|---|
| Lower Back Pain | Affects daily comfort |
| Numbness/Tingling | Sensory disturbances in legs |
| Weakness | Difficulty with mobility |
As these symptoms progress, you’ll likely find walking increasingly difficult. This can lead to a decline in overall coordination, making everyday activities more taxing. It’s not uncommon for lumbar myelopathy to also affect bowel or bladder function, adding another layer of complexity to the condition.
Ignoring these signs can worsen symptoms over time, so it’s important to stay vigilant. Seeking medical advice early can help manage these symptoms and prevent further complications. Remember, timely intervention can make a significant difference in maintaining your quality of life.
Related Article: Elbow Injury: Causes, Treatment, and Recovery Tips
Causes of Lumbar Myelopathy

When considering the causes of lumbar myelopathy, you should be aware that spinal stenosis is a common culprit, as it narrows the spinal canal and compresses the cord.
Degenerative diseases like arthritis or disc degeneration also play a significant role, gradually impacting the spine’s structure.
Additionally, trauma or injury to the lumbar spine can lead to this condition, highlighting the risks associated with physical damage.
Common Causes Unveiled
Understanding the causes of lumbar myelopathy is essential for effective diagnosis and treatment. Often, lumbar myelopathy arises from spinal stenosis, where the spinal canal narrows, compressing the spinal cord. Herniated discs can also exert pressure on the spinal cord, leading to similar symptoms. Degenerative changes in the spine, such as arthritis or disc degeneration, are common culprits that gradually wear down the protective structures of your spine. These changes can significantly contribute to lumbar myelopathy by altering the spine’s normal function.
Beyond degenerative issues, spinal cord injuries from trauma or accidents can instantly cause lumbar myelopathy. Congenital abnormalities or malformations present from birth might also predispose you to developing this condition. Infections like spinal abscesses or meningitis can inflame the spinal cord area, resulting in myelopathy. Even though less common, these infections can be severe and require immediate attention.
Autoimmune disorders such as rheumatoid arthritis or lupus may also play a role. They can cause inflammation and damage in the lumbar region, leading to myelopathy. By understanding these causes, you can better anticipate potential risks and work closely with your healthcare provider to effectively manage or prevent lumbar myelopathy.
Degenerative Disease Impact
Degeneration is an unyielding adversary in the battle against lumbar myelopathy. You’re up against degenerative diseases like spinal stenosis, disc herniation, and arthritis, which can greatly affect your lower spine. These conditions contribute to changes such as bone spurs and disc degeneration. Over time, wear and tear can lead to the narrowing of the spinal canal, resulting in spinal cord compression.
Here’s a quick breakdown of how these degenerative changes might affect you:
| Condition | Impact on Spine | Potential Outcome |
|---|---|---|
| Spinal Stenosis | Constriction of the spinal canal | Spinal cord compression |
| Disc Herniation | Protrusion of disc material | Nerve pressure, pain |
| Arthritis | Joint swelling | Increased bone spurs |
| Bone Spurs | Irregular bone growth | Narrowing of nerve pathways |
| Wear and Tear | Overall deterioration over time | Chronic pain, mobility issues |
These degenerative processes can predispose you to lumbar myelopathy as you age, making everyday activities challenging. Conditions like spondylosis and degenerative disc disease also play a role, gradually wearing down your spine’s integrity. Understanding these factors is essential in managing the progression and impact of lumbar myelopathy on your life. Stay informed and consult with healthcare professionals to explore appropriate interventions.
Trauma and Injury Risks
While degenerative diseases greatly contribute to lumbar myelopathy, trauma and injury pose equally serious risks. You mightn’t realize it, but traumatic injuries from car accidents, falls, or sports-related impacts can lead directly to this debilitating condition. When these incidents occur, they can cause fractures and dislocations, putting immense pressure on your lumbar spine. This, in turn, might result in spinal cord contusions, which are bruises on the spinal cord, leading to myelopathy.
Imagine a situation where you experience a high-impact trauma to your lumbar spine, like falling from a substantial height. Such an event can forcefully compress or twist your spinal cord, significantly heightening the risk of developing lumbar myelopathy. These injuries often happen suddenly, leaving little room for prevention and requiring immediate attention.
Understanding the specific mechanism of your injury is essential. It not only helps in diagnosing lumbar myelopathy but also guides the treatment plan. If you’re aware of the risks associated with these traumatic injuries, you can take proactive measures to protect your spine.
Whether wearing a seatbelt, using protective gear in sports, or being cautious with heights, prevention is always better than cure.
Diagnosing Lumbar Myelopathy
When diagnosing lumbar myelopathy, you’ll rely on key diagnostic tests like X-rays, MRIs, and CT scans to view the spine and spinal cord.
Recognizing symptoms and indicators early is important, as electrical studies such as EMGs help assess nerve function and prevent permanent damage.
Early detection through these tests is crucial for effective treatment planning and better outcomes.
Key Diagnostic Tests
A thorough examination often involves a blend of imaging and nerve function tests to guarantee precision in diagnosing lumbar myelopathy. X-ray imaging can be your first step, providing an initial look at the spine and helping rule out other conditions. While X-rays are helpful, they don’t offer detailed views of the spinal cord. That’s where Magnetic Resonance Imaging (MRI) comes into play.
As a key diagnostic tool, an MRI gives you a detailed image of the spinal cord, helping identify any compression or abnormalities associated with lumbar myelopathy. It’s vital for pinpointing the exact location and extent of the problem.
Electromyography (EMG) is another significant test that evaluates nerve function. By considering the electrical activity in your muscles, EMG provides insight into how well your nerves are working, offering additional clues to diagnose lumbar myelopathy. Combining MRIs and EMG, this thorough approach ensures early and accurate diagnosis, which is fundamental for planning effective treatment strategies.
Symptoms and Indicators
Recognizing the symptoms of lumbar myelopathy is important for early intervention and effective management. When lumbar myelopathy occurs, it can manifest in various ways that you need to be aware of. Symptoms of lumbar myelopathy often include pain in the lower back and legs.
You might experience a loss of sensation, numbness, or tingling in your lower extremities. This can be unsettling and may hinder your daily activities significantly.
Weakness in the legs is another common indicator, making it difficult for you to walk or maintain your balance. These symptoms shouldn’t be ignored, as they could indicate nerve damage.
Pay attention to any changes in bowel or bladder function, as these are also important signs. Such changes can be embarrassing and disruptive, suggesting that the condition might be progressing.
If you’re noticing these symptoms, seeking a healthcare provider’s evaluation is essential. They’ll likely recommend imaging tests like an MRI to visualize your spinal cord and nerve conduction studies to assess nerve function.
Electromyography (EMG) can also help pinpoint nerve damage, aiding in an accurate diagnosis. Addressing these symptoms promptly can prevent further complications.
Importance of Early Detection
Detecting lumbar myelopathy early is essential to prevent irreversible nerve damage. You need to recognize symptoms like back pain, numbness, and weakness, which can be key indicators of this condition. Please don’t ignore these early signs; they signal the need for prompt diagnosis. By seeking timely intervention, you can relieve symptoms and improve outcomes significantly.
Consulting a spine specialist is necessary to diagnose and manage lumbar myelopathy accurately. These specialists have the expertise to conduct thorough evaluations and recommend the right diagnostic tests. Tests like MRI and electromyogram are crucial in confirming lumbar myelopathy, helping guide your treatment decisions.
With early detection, you can avoid permanent nerve damage and maintain your quality of life.
Nonsurgical Treatment Options

When exploring nonsurgical treatment options for lumbar myelopathy, you’ll find several effective approaches to enhance your quality of life greatly. Medication is a common first step, helping to manage pain and inflammation associated with this condition. By reducing discomfort, you can engage more fully in other treatments.
Physical therapy is essential in improving mobility, strength, and function. A tailored exercise program can help you regain movement and support spinal health. Bracing may be recommended to provide additional support to your spine, reducing pressure on the spinal cord and potentially alleviating symptoms.
Corticosteroid injections offer another nonsurgical treatment option, targeting inflammation and swelling. These injections can provide significant relief from discomfort and improve function. Alongside medical interventions, lifestyle modifications are equally important.
Maintaining a healthy weight can lessen the load on your spine while avoiding activities that worsen your symptoms, which can help you manage your condition more effectively. Incorporating these changes into your daily routine can substantially affect how you feel and function. Considering these nonsurgical approaches, you can proactively manage lumbar myelopathy and improve your overall well-being.
Surgical Treatment Options
For those dealilumbar myelopathy, surgical treatment options offer a more direct approach to addressing the condition. If non-surgical methods don’t improve your oms or significant nerve compression is present, surgery might be recommended. One common procedure is spinal decompression surgery, which aims to relieve pressure on your theal cord. This can help alleviate symptoms and prevent further damage. Another option is laminoplasty, which widens the spinal canal to ease nerve compression.
The choice of surgery depends on how severe your symptoms are and the specifics of your spinal condition. Understanding these procedures can help you make informed decisions.
Here’s a quick comparison of surgical options:
| Procedure | Purpose | Benefits |
|---|---|---|
| Spinal Decompression | Relieve pressure on the spinal cord | Alleviates symptoms |
| Laminoplasty | Widen the spinal canal | Eases nerve compression |
| Fusion Surgery | Stabilize affected vertebrae | Prevents further deterioration |
| Diskectomy | Remove herniated disk material | Reduces nerve irritation |
| Laminectomy | Remove part of vertebrae | Increases spinal canal space |
Surgical intervention addresses the underlying cause of lumbar myelopathy, offering relief and maintaining your spinal health.
When to Consult a Specialist

After exploring surgical treatment options, knowing when to consult a specialist about lumbar myelopathy becomes crucial. If you experience weakness, numbness, or difficulty walking in your lower back or legs, reaching out to a spine specialist is vital. These symptoms might indicate a deterioration of the condition, and receiving specialized care can make a significant difference.
If you’ve been diagnosed with lumbar myelopathy, seeking expert advice will help you grasp the range of treatment options available and what might work best for you.
Early consultation can lead to better management of your symptoms and improve overall outcomes. A spine specialist has the expertise to effectively diagnose and treat lumbar myelopathy. They can provide customized treatment plans to alleviate symptoms and prevent further progression.
Being proactive is crucial. If symptoms worsen or if new symptoms develop, don’t a specialist promptly. Timely evaluation and care are vital in managing lumbar myelopathy.
Finding a Spine Specialist
To effectively manage lumbar myelopathy, finding the right spine expert is vital. A qualified spine doctor can offer expert care and develop personalized treatment plans that address your condition and symptoms. Start by locating a spine expert near you to guarantee convenient access to care.
Research the qualifications and experience of potential experts. Look for those with a proven track record in treating lumbar myelopathy. Their expertise should align with your particular needs, ensuring they understand the complexities of your condition. This expertise is essential in crafting treatment plans that cater to your symptoms.
Healthcare providers and trusted sources can be valuable when choosing a spine expert. They may offer recommendations based on their knowledge of the specialist’s reputation and success in similar cases. Don’t hesitate to ask them for referrals.
Ensure the spine expert you choose thoroughly understands lumbar myelopathy, from diagnosis to treatment. This guarantees that any plan they propose is tailored to your unique situation. Taking these steps will help you find a spine expert who can guide you through managing your condition effectively and confidently.
Long-term Management Strategies

Effective long-term management of lumbar myelopathy requires regular monitoring, lifestyle changes, and professional guidance. You’ll need to keep up with regular follow-up appointments to stay on top of your condition. These check-ins allow for monitoring symptoms and making necessary adjustments to your treatment plan.
Physical therapy and exercise programs are pivotaltaining mobility and function. By working with a physical therapist, you can develop a personalized exercise routine that targets your specific needs and helps prevent further decline.
Lifestyle modifications are equally important. Maintaining a healthy weight reduces stress on your spine, while proper posture can alleviate pressure on affected areas. These changes can greatly impact your overall well-being and are crucial components of long-term management for lumbar myelopathy.
Collaboration with a multidisciplinary team is essential. You’re ensuring thorough care by engaging with physical therapists, pain specialists, and surgeons. Each specialist offers unique insights and expertise, optimizing your treatment approach.
Frequently Asked Questions
Is Lumbar Myelopathy Serious?
You should know it can be serious—symptThe progression of symptomscts long-term outcomes. Treatment options, including non-surgical therapies and rehabilitation strategies, impact prognosis factors. Surgical risks exist, but timely intervention improves outcomes. Act early for better results.
What Is the Life Expectancy of Someone With Myelomalacia?
You’re wondering about life expectancy with myelomalacia. Symptoms and progression vary, but treatment options like surgical intervention and physical therapy can improve prognosis and recovery. Risk factors influence the long-term outlook, so work with doctors for the best outcomes.
What Is One Cause of Myelopathy?
You might wonder about the causes. Degenerative disc issues and spinal stenosis often play a role. Trauma-related injuries, tumor compression, inflammatory diseases, or genetic predisposition can also lead to it. Surgical options usually offer relief.
How Do You Diagnose Myelopathy?
To diagnose myelopathy, you assess symptoms and perform a physical exam. Imaging studies, electromyography, and nerve conduction studies help. Consider differential diagnosis before discussing treatment options and evaluating prognosis for an accurate and effective diagnosis.
Conclusion
You’ve learned that lumbar myelopathy is a serious condition requiring attention and timely intervention. Recognizing symptoms like pain, numbness, and weakness is important. By understanding its causes and seeking early diagnosis through X-rays or MRIs, you can explore treatment options from physical therapy to surgical procedures. Collaborating with a multidisciplinary team guarantees thorough care, helping you manage symptoms and improve your quality of life. Don’t hesitate to consult a specialist when needed.

