You’re probably aware that back pain is a common issue, but did you know that females often experience unique challenges when it comes to this discomfort? From hormonal fluctuations to anatomical differences, these factors can greatly impact your spine health. It’s important to understand how conditions like endometriosis or osteoporosis might contribute to your pain. Have you considered how your posture or core strength might play a role in managing these symptoms? Understanding these connections could be the key to effective pain management, but what specific strategies should you be focusing on?
Key Takeaways
- Hormonal fluctuations and post-menopausal changes can intensify back pain in women.
- The female pelvis and smaller sacroiliac joints affect lumbar spine alignment, impacting back pain.
- Endometriosis and degenerative spondylolisthesis are common causes of lower back pain in women.
- Osteoporosis and osteoarthritis are prevalent in women over 50, contributing to spinal issues.
- Ergonomic practices and core strengthening exercises are essential for preventing back pain.
Causes of Female Back Pain

Understanding the reasons behind female back pain is vital for effective management and prevention. Women often experience persistent back pain due to a variety of factors. One important factor is hormonal fluctuations, which can worsen spinal conditions. For example, post-menopausal women are more prone to conditions like osteoarthritis and osteoporosis, where bones become fragile and joints deteriorate, increasing the risk of persistent back pain.
Lower back pain in women can also arise from anatomical variances. A broader pelvis and smaller sacroiliac joints can impact the alignment of the lumbar spine, leading to discomfort and pain.
Moreover, endometriosis, a condition where tissue resembling the lining inside the uterus grows outside it, is a common cause of lower back pain. This can be debilitating, contributing significantly to enduring pain.
Spinal conditions such as degenerative spondylolisthesis, where one vertebra slips over the one below it, are also common among women, causing ongoing back pain. Additionally, organs like the kidneys, uterus, and ovaries can be sources of pain due to conditions like kidney infections and fibroids. Recognizing these factors is essential in addressing and managing back pain effectively.
Common Conditions in Women
When it comes to common conditions affecting women’s back health, several specific disorders stand out. Lower back pain is often linked to endometriosis, impacting 190 million women globally. This gynecological disorder frequently causes discomfort in the lower back. As women age, spinal osteoarthritis becomes more prevalent. This condition, common in women over 50, results from hormonal changes leading to inflammation and bone spurs that irritate nerves.
| Condition | Common Age Group | Symptoms |
|---|---|---|
| Endometriosis | Reproductive Age | Lower back pain |
| Spinal Osteoarthritis | 50+ | Nerve irritation, inflammation |
| Spinal Osteoporosis | Post-Menopause | Compression fractures, kyphosis |
| Degenerative Spondylolisthesis | 50+ | Stiffness, spasms, neurological issues |
| Piriformis Syndrome | All Ages | Lower back/gluteal pain, tingling |
Spinal osteoporosis, four times more common in women, weakens bones post-menopause, leading to compression fractures and kyphosis. Degenerative spondylolisthesis, also more frequent in women over 50, involves vertebra slippage causing stiffness and muscle spasms. Piriformis syndrome, affecting more women than men, involves the piriformis muscle pressing on the sciatic nerve, leading to gluteal and lower back pain, with tingling in the buttocks and thighs. Understanding these conditions can help you take proactive measures to manage back health effectively.
Anatomy and Back Pain
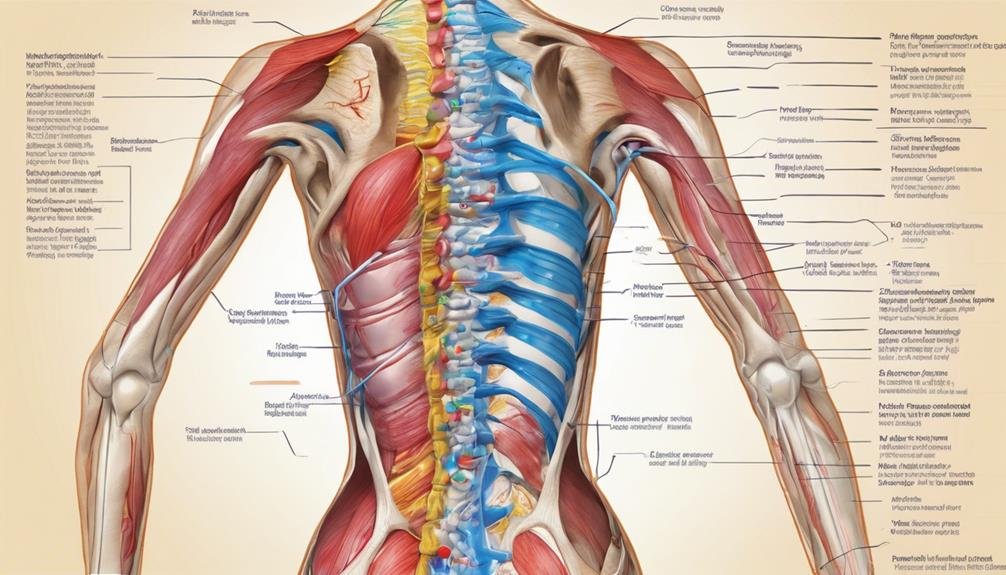
When you consider anatomy’s role in back pain, the female pelvis, sacroiliac joints, and lumbar spine alignment are key factors.
A wider pelvis can affect how your lumbar spine aligns, leading to discomfort.
Also, smaller sacroiliac joints can increase strain, making it essential to understand these influences to address back pain effectively.
Female Pelvis Influence
The anatomy of the female pelvis plays a significant role in influencing back pain. With a broader pelvic structure, your lumbar spine alignment can be impacted, potentially leading to back pain issues. This distinct shape of the female pelvis affects how pressure is distributed across your lower back, sometimes causing discomfort or strain. The smaller sacroiliac joints in women also play an essential role, as they can struggle to adequately support the lumbar region, leading to further back pain problems. Understanding these aspects of female anatomy can help you identify specific alignment and support challenges that might contribute to your discomfort.
Your pelvis’s structure directly influences how your spine aligns and supports your back. Since women have a naturally broader pelvis, this can cause the lumbar spine to shift slightly, creating additional pressure on certain areas. This pressure distribution may not only lead to discomfort but also exacerbate existing back pain issues.
Sacroiliac Joint Strain
In understanding back pain, it’s essential to look at the sacroiliac joint, which connects your sacrum to your pelvis. This joint plays a pivotal role in providing stability and absorbing shock in your lower back. When the sacroiliac joint experiences strain, it can lead to significant lower back pain. This strain often results from factors like trauma, pregnancy, arthritis, or repetitive stress. You’ll typically feel pain in the lower back, buttocks, and thighs, especially when walking or standing.
To effectively address sacroiliac joint strain, consider these steps:
- Diagnosis: Start with a physical examination. Your doctor may use imaging tests or diagnostic injections to confirm the source of your pain.
- Treatment: Physical therapy is often recommended to strengthen the muscles around the joint, improving stability and reducing pain. Medications or injections may also help manage discomfort.
- Advanced Solutions: In severe cases, surgery might be necessary to stabilize the joint and alleviate chronic pain.
Lumbar Spine Alignment
Sacroiliac joint strain isn’t the only factor contributing to back pain in women; lumbar spine alignment plays a significant role too.
The unique aspects of female anatomy, particularly the wider pelvic structure, can lead to changes in how your lumbar spine aligns. This alignment difference often results in increased strain on your lower back, which might cause discomfort or more severe back pain over time.
Understanding the impact of your pelvic structure on lumbar spine alignment is essential for maintaining back health. With a wider pelvis, there’s a tendency for your spine to bear additional pressure, especially since women’s sacroiliac joints are generally smaller. This added pressure can exacerbate strain and lead to persistent back issues if not addressed properly.
Proper pelvic alignment and lumbar spine alignment are vital in reducing strain and ensuring your back remains healthy. Paying attention to these anatomical differences can help you take proactive steps to prevent back pain. Engaging in exercises that strengthen your core and promote better posture can alleviate some of the pressure on your spine, improving your overall back health and reducing the risk of chronic pain.
Hormonal Factors
You might notice how hormonal fluctuations can intensify back pain, especially during menstrual cramps and conditions like endometriosis. Estrogen plays an important role in maintaining bone strength, and its decline post-menopause can lead to spinal issues such as osteoporosis. Understanding these hormonal factors can help you better manage back pain specific to women.
Hormonal Fluctuations and Pain
Hormonal fluctuations play a significant role in contributing to back pain in women. These fluctuations can lead to conditions like spinal osteoarthritis and endometriosis, causing significant discomfort.
During the menstrual cycle, hormonal changes can trigger lower back pain, especially if you experience endometriosis or painful menstruation. Moreover, estrogen decline post-menopause increases the risk of spinal osteoporosis, weakening bones and causing potential height loss.
Understanding these hormonal factors is essential for managing back pain effectively, as they can uniquely impact your female anatomy, influencing the alignment of the lumbar spine and increasing strain on the sacroiliac joints.
Consider these key points:
- Hormonal Changes and Conditions: Hormonal fluctuations can exacerbate spinal osteoarthritis and endometriosis, leading to increased back pain.
- Menstrual Cycle Impact: The menstrual cycle can trigger lower back pain due to endometriosis or painful menstruation, emphasizing the need for targeted pain management strategies.
- Post-Menopause Concerns: With estrogen decline, there’s a higher risk of spinal osteoporosis, which can weaken bones and affect spinal alignment, contributing to back pain.
Estrogen’s Role in Back Pain
Estrogen plays a central role in back pain experienced by many women, influencing both the intensity and frequency of discomfort. You might notice that during your menstrual cycle, hormonal changes can worsen back pain symptoms. This fluctuation in estrogen levels can lead to variations in how strong or frequent your back pain feels. It’s crucial to recognize this pattern as it can help tailor treatment approaches specifically for you.
After menopause, estrogen levels drop significantly, which can contribute to increased back pain. This decrease affects your bone density, making your spine more vulnerable to issues that can cause pain. Maintaining good spinal health post-menopause becomes essential to managing discomfort. Estrogen’s role in maintaining bone density is important, as a decline can lead to conditions like osteoporosis, further impacting your spinal health.
Understanding the link between estrogen and back pain helps in devising better strategies to alleviate discomfort. Whether it’s through hormonal therapies or lifestyle changes, recognizing these hormonal factors allows you to take proactive steps in managing back pain effectively. By being aware of how estrogen impacts your body, you can work towards minimizing its adverse effects on your spinal health.
Symptoms Requiring Attention

When experiencing back pain, it’s essential to recognize symptoms that need immediate medical attention. Ignoring these signs could lead to worsening conditions or permanent damage. Some symptoms demand urgent attention due to their serious implications.
- Loss of Bowel or Bladder Control: This alarming symptom may indicate cauda equina syndrome, a form of nerve damage that requires immediate medical intervention. Time is vital here; seeking help promptly can prevent irreversible harm.
- Radiating Numbness, Tingling, or Pain: If you notice these sensations in your arms or legs, it’s a warning sign that shouldn’t be ignored. These symptoms can suggest potential nerve damage, and early evaluation is essential to prevent further complications.
- High Fever with Back Pain: A fever paired with back pain might be more than a simple infection. It could signal a spine infection, which needs urgent medical treatment. Don’t wait to get checked out if these symptoms appear together.
Pay attention to these crucial symptoms, and don’t hesitate to seek medical advice if you experience any of them. Quick action can make a significant difference in preventing further health issues. Always err on the side of caution when it comes to your health.
Pain Management Techniques
Finding effective ways to manage back pain can significantly improve your quality of life. Start by exploring acupuncture, which can relieve pain by targeting specific points in your body. Incorporating mindfulness meditation into your routine helps to reduce stress and improve your mental health, which is vital in pain management. Pay attention to your posture; correct posture adjustments prevent unnecessary strain on your back.
Exercise is another key component. It strengthens the muscles supporting your spine and boosts your overall well-being. Choose activities that suit your abilities, and consider options like yoga, which doubles as an exercise and an alternative therapy.
Don’t underestimate the power of nutrition; a balanced diet rich in calcium, vitamin D, and omega-3 fatty acids supports your back health.
For more immediate relief, explore medical treatments such as NSAIDs and muscle relaxants. Physical therapy is also a viable option, offering personalized care to address your specific pain points. Additionally, alternative therapies like chiropractic care and aquatic therapy can provide relief and enhance your flexibility.
Tailoring these techniques to your needs can help you manage back pain effectively and enhance your daily life.
Preventative Measures

Alongside managing existing back pain, consider adopting preventative measures to reduce future discomfort. To effectively prevent back pain, focus on making proactive adjustments in your daily routine. Implement ergonomic practices at work and home to minimize strain. Adjust your chair, desk, and computer setup to support proper posture and reduce the risk of developing chronic pain. Strengthening your core muscles through regular exercise can also be a key preventive measure. Core exercises enhance your stability and support your spine, reducing the chance of future discomfort.
Here are three actionable steps you can take:
- Exercise Regularly: Engage in exercises that strengthen your core muscles and improve your overall mental health, contributing to back pain prevention.
- Practice Good Posture: Be mindful of your posture whether sitting or standing. Ergonomic practices, like adjusting your workspace, can notably reduce strain on your back.
- Maintain a Balanced Diet: Dietary support is important. Consume foods rich in calcium, vitamin D, lean proteins, and omega-3 fatty acids to bolster your back health.
Frequently Asked Questions
What Causes Lower Back Pain in a Woman?
You might experience lower back pain due to hormonal imbalances, pregnancy complications, or menstrual cycle fluctuations. Poor posture, osteoporosis risk, pelvic inflammatory disease, and endometriosis symptoms can also contribute to discomfort in your lower back.
What Are the Red Flags for Back Pain?
You should look for red flags like loss of bladder control or severe weakness. Early detection of symptoms through diagnostic tests like imaging is vital. Treatment options and preventive measures, including exercises, help manage chronic pain and its impact.
How Do I Know if My Back Pain Is a Disc or Muscle?
To determine if your back pain is disc vs muscle, notice how symptoms differ: radiating vs dull pain. Diagnostic tests like MRI help. Treatment includes physical therapy, lifestyle changes, and preventing re-injury. Explore specific treatment options.
What Organ Would Cause Pain in the Right Side of the Back?
You might experience right-side back pain due to kidney stones, gallbladder issues, or appendicitis symptoms. Ovarian cysts, uterine fibroids, endometriosis pain, or pancreatitis pain can also cause discomfort. Consult a doctor for a proper diagnosis.
Conclusion
Understanding the unique causes of back pain in women helps you manage your discomfort more effectively. Pay attention to hormonal changes, spine alignment, and conditions like endometriosis or osteoporosis. If you notice persistent or severe symptoms, don’t hesitate to seek medical advice. Focus on strengthening your core muscles, practice good posture, and consider preventative measures. By staying proactive and informed, you’re better equipped to address and alleviate your back pain.

