When you think about pain, you might picture a sharp cut or a sprained ankle, but visceral pain is a different beast altogether. It comes from your internal organs, creating a dull and often confusing sensation that’s tough to pinpoint. Imagine feeling discomfort that’s not just confined to one area, but seems to echo throughout your body. This type of pain often brings along unexpected companions like nausea or a fever, making diagnosis tricky. So, why is understanding visceral pain so vital, and what hidden messages could your body be sending you through these sensations?
Key Takeaways
- Visceral pain originates from internal organs and is often diffuse, dull, and hard to localize.
- It can involve referred pain, making diagnosis challenging and complicating symptom identification.
- Common causes include conditions like IBS, IBD, cancer, and pancreatitis.
- Diagnosis often requires medical history, physical exams, and imaging studies like CT scans or MRIs.
- Treatment may include medications, lifestyle changes, and alternative therapies like acupuncture and yoga.
Understanding Visceral Pain

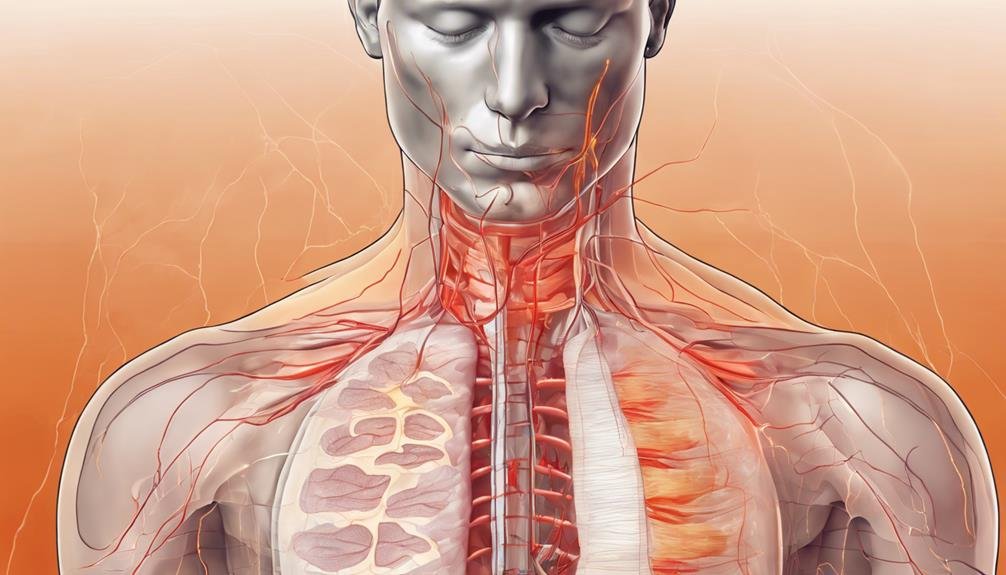
When it comes to understanding visceral pain, it’s important to recognize that this type of pain originates from your internal organs like the heart, lungs, and reproductive system. You might notice that visceral pain often presents as dull, aching sensations that are notoriously hard to pinpoint. This makes it difficult to identify the exact source of discomfort, adding to the complexity of diagnosing the underlying issue.
One of the significant characteristics of visceral pain is referred pain. This is when you feel pain in a different area from where it originates, which complicates diagnosis. For instance, you might experience shoulder pain when the real problem lies within your gallbladder. These nuances make understanding visceral pain a bit of a challenge.
Common examples of visceral pain include menstrual cramps and urinary tract infections. Both can manifest as deep, aching sensations that don’t always provide clear clues about their origins. Because of this, it can be tough to determine the precise cause without further investigation.
Recognizing these characteristics is key to addressing and managing visceral pain effectively, even though the path to a conclusive diagnosis can be challenging.
Visceral Vs. Somatic Pain
Distinguishing between visceral and somatic pain is vital for accurate diagnosis and treatment. Visceral pain is often diffuse, dull, and aching, which makes it tricky to pinpoint. Unlike somatic pain, which is sharp and localized, visceral pain can be accompanied by nonspecific symptoms. This diffuse nature means it’s more challenging to diagnose correctly, requiring a deeper understanding of the nuances between visceral vs. somatic pain.
The localized nature of somatic pain, however, often results in a more straightforward diagnosis.
Importantly, mental health conditions like anxiety and depression are frequently associated with chronic visceral pain. This connection is less common with somatic pain. The persistent discomfort and uncertainty linked to visceral pain can exacerbate these mental health conditions, creating a cycle that affects your overall well-being.
Recognizing this relationship is crucial for developing an appropriate treatment plan that addresses both physical and emotional aspects.
Causes of Visceral Pain

Understanding the causes of visceral pain is essential to effectively manage and treat this complex condition. Visceral pain causes are often linked to underlying health issues affecting your internal organs. Conditions like IBD (Inflammatory Bowel Disease) and IBS (Irritable Bowel Syndrome) commonly trigger visceral pain, leading to discomfort in your digestive tract. Serious illnesses such as cancer and pancreatitis can also be culprits, where tumors or inflammation can disrupt normal organ function.
Indigestion might seem minor, but it can cause significant visceral pain, especially if it indicates a deeper problem. Interstitial cystitis, a chronic condition affecting the bladder, is another source of visceral pain you might experience. Sometimes, life-threatening situations like heart attacks or bowel obstructions can cause intense and immediate visceral pain, signaling that you need urgent medical intervention.
Pain from these conditions occurs because pain receptors in your visceral organs are less densely packed and more spread out, making it hard to pinpoint. This diffuse sensation means visceral pain often indicating significant health concerns. Therefore, recognizing its causes through thorough diagnostic evaluation is essential to make sure you receive the appropriate treatment and care promptly.
Symptoms and Characteristics
When you’re experiencing visceral pain, you’ll typically notice a diffuse and dull sensation that makes it hard to pinpoint the exact source.
You might also encounter referred pain, where discomfort appears in a different area than where it originates.
Additionally, be aware of autonomic response indicators like changes in heart rate, blood pressure, sweating, and nausea that often accompany this type of pain.
Diffuse and Dull Sensations
One might find visceral pain particularly perplexing, as it manifests as diffuse and dull sensations that are hard to pinpoint. This type of discomfort often originates from internal organs such as the abdomen or pelvis, presenting as a deep aching or twisting discomfort. You might experience it as gnawing pain, or even colicky pain, with an intensity that can vary from mild to severe. The challenge lies in its nonspecific symptoms, which might include nausea or sweating, making it difficult to distinguish from other ailments.
Unlike somatic pain, which is sharp and localized, visceral pain lacks this clarity, adding to the complexity of diagnosing its source.
Here are some feelings you might experience with visceral pain:
- Confusion: The diffuse sensations make it hard to identify what’s wrong.
- Frustration: The dull discomfort lingers, and relief seems elusive.
- Anxiety: The deep ache raises concerns about your internal organs.
- Helplessness: The twisting discomfort feels beyond your control.
- Isolation: The gnawing pain can make you feel misunderstood.
Referred Pain Phenomenon
The enigma of referred pain often leaves both patients and practitioners puzzled, as this phenomenon involves feeling discomfort in areas far removed from the actual source of the problem. Referred pain occurs due to shared nerve pathways, which can cause visceral pain to manifest in unexpected, remote areas of your body. This can make diagnosis quite challenging, as the pain experienced doesn’t necessarily align with the location of the underlying issue.
For example, you might feel shoulder pain during a heart attack or experience back pain from a kidney infection. These symptoms can confuse both you and your healthcare provider, potentially delaying accurate diagnosis and treatment. Understanding referred pain patterns becomes essential in such scenarios, enabling healthcare providers to look beyond the obvious and consider underlying visceral pain issues.
Recognizing these patterns helps them accurately pinpoint the source of discomfort and address the root cause rather than just the symptoms. By acknowledging the complexities of referred pain, you and your healthcare provider can work together more effectively, ensuring a more precise diagnosis. As you navigate these challenges, remember that understanding referred pain is a vital step in managing your health effectively.
Autonomic Response Indicators
Referred pain’s intricate patterns can often mask the true source of discomfort, but paying attention to autonomic response indicators offers another layer of insight into visceral pain. When your body experiences visceral nociception, the autonomic nervous system springs into action. This results in various autonomic responses, including changes in heart rate and blood pressure.
You might notice increased sweating, as the body attempts to cope with the internal distress. It’s not uncommon to experience nausea and pallor, as these symptoms signal the body’s internal response to visceral pain.
Monitoring these autonomic indicators can provide valuable insights into how visceral pain affects you physiologically. Pay attention to fluctuations in essential signs, like heart rate variability and alterations in blood flow. These subtle clues are your body’s way of communicating its struggle.
- Fear: The unexpected surge in symptoms can create anxiety.
- Confusion: Misinterpreting these signs might lead to panic.
- Relief: Understanding them can offer clarity and control.
- Helplessness: When symptoms feel overwhelming.
- Hope: Recognizing these can lead to better pain management.
Diagnosis of Visceral Pain
Diagnosing visceral pain often demands a thorough approach to ensure accuracy and effectiveness. Begin by providing a detailed medical history, which assists your healthcare provider in understanding the context of your pain. During the physical examination, they’ll evaluate associated symptoms and identify potential pain sources. A differential diagnosis is essential here, as it helps eliminate other possible conditions that might resemble visceral pain.
Imaging studies, such as CT scans or MRIs, play a substantial role in identifying structural abnormalities in your organs. These scans offer detailed views that can spotlight issues contributing to your pain. Endoscopic procedures may also be required. They allow direct visualization of your internal organs, offering insights into conditions that could be causing discomfort.
Blood tests are another vital diagnostic tool. They’ll examine for markers of inflammation or infection, which can greatly assist in pinpointing the cause of your visceral pain. Identifying these markers helps in understanding whether inflammation or an infection is involved, potentially guiding further treatment.
Related Article: Understanding and Managing Knee Spasms for Optimal Health
Treatment Options
When dealing with visceral pain, you’ll find that treatment often starts with medications like NSAIDs, acetaminophen, or even prescription options such as gabapentin and opioids.
Beyond medications, embracing lifestyle changes and exploring alternative therapies like physical therapy and relaxation techniques can greatly help manage your pain.
In certain situations, more intensive options like surgery or nerve blocks might be necessary, highlighting the importance of a personalized and thorough approach to your care.
Medications and Therapies
Managing visceral pain often involves a combination of medications and therapies tailored to your needs. You might start with nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or acetaminophen to ease discomfort. If pain persists, your doctor could prescribe gabapentin or pregabalin, especially for chronic cases. These medications work by altering the way your nerves send pain signals, providing relief.
In addition to medications, physical therapy can play an essential role in managing visceral pain. By incorporating exercises and relaxation techniques, you can improve your body’s ability to cope with pain.
For more challenging cases, nerve blocks or surgical interventions might be necessary when other treatments aren’t effective.
Alternative therapies, such as acupuncture, massage, and yoga, offer additional avenues for relief, helping you tackle pain from different angles.
Dealing with visceral pain can be overwhelming, but you’re not alone:
- Hope: Relief is possible with the right treatment plan.
- Empowerment: You have options and control over your pain management.
- Support: Therapies and medications work together to support your healing.
- Resilience: Every small step counts in your journey to recovery.
- Relief: Feel the burden of pain lifted, paving the way for a brighter future.
Lifestyle and Alternative Approaches
A holistic approach to managing visceral pain often includes lifestyle and alternative strategies that can make a noteworthy difference. By incorporating lifestyle modifications, you can markedly alleviate symptoms. Start with stress management techniques, such as meditation and yoga, which promote relaxation and reduce stress, a well-known trigger for visceral pain.
Regular exercise and ensuring you get adequate sleep also play pivotal roles in managing your discomfort.
Exploring alternative approaches like acupuncture can also provide relief. Acupuncture has been shown to ease pain by releasing endorphins and improving energy flow in the body.
Meanwhile, dietary changes, particularly adopting a low-inflammatory diet rich in fruits, vegetables, and whole grains, can support overall health and potentially reduce visceral pain.
Physical therapy is another excellent option. It helps improve posture, strengthens core muscles, and decreases bodily tension—all essential for managing visceral pain effectively.
Additionally, mind-body techniques such as biofeedback and cognitive-behavioral therapy enhance awareness and promote relaxation, helping you cope better with your pain.
Alternative Therapies

Exploring alternative therapies for visceral pain can offer a valuable complement to traditional medical treatments. These approaches, such as acupuncture, massage therapy, yoga, TENS, and neuromuscular therapy, can help you manage symptoms and improve your overall well-being. Acupuncture, for instance, involves inserting thin needles at specific points to alleviate pain and promote healing.
Meanwhile, massage therapy works to relax muscles, improve circulation, and reduce tension associated with visceral pain.
Yoga not only enhances flexibility but also promotes relaxation, helping you find relief from discomfort. TENS, or transcutaneous electrical nerve stimulation, uses low-voltage electrical currents to relieve pain and is a popular choice for many seeking non-invasive solutions. Neuromuscular therapy focuses on releasing muscle spasms and improving the balance between the nervous and muscular systems.
Consider these options to support your journey:
- Empowerment: Regain control over your body and pain.
- Hope: Discover new ways to improve your quality of life.
- Relief: Experience moments of calm and relaxation.
- Comfort: Find solace in therapies tailored to your needs.
- Resilience: Build strength through holistic approaches.
Current Research Trends
Recent advancements in the study of visceral pain are changing how we perceive and address chronic pain in the body’s internal organs. Researchers are delving into the intricate mechanisms that cause this type of chronic pain, using cutting-edge neuroimaging techniques. These techniques are giving us a clearer picture of how the brain processes and responds to visceral pain stimuli, offering hope for more effective interventions.
Current research is also focusing on targeted drug development to reduce pain sensitivity. By honing in on specific pathways, new medications could improve the quality of life for those suffering from visceral pain.
In addition, multidisciplinary approaches are becoming increasingly crucial. Pain specialists, psychologists, and physiotherapists work together to create thorough pain management strategies tailored to individual needs.
Patient-centered care is at the heart of these strategies, emphasizing shared decision-making between you and your healthcare team. This approach guarantees that your personal experiences and preferences are considered, leading to more effective and satisfactory outcomes. By integrating these elements, the latest research trends aim to provide you with a well-rounded, efficient approach to managing visceral pain, making it simpler to regain control over your life.
Frequently Asked Questions
What Is a Visceral Pain?
You’re experiencing discomfort deep within your internal organs. Sensations vary, often dull and hard to pinpoint. Causes include acute episodes or chronic conditions, affecting the nervous system. Diagnosis, treatment, and management strategies can mitigate symptoms and emotional impact.
What Is the Difference Between Muscle Pain and Visceral Pain?
You differentiate muscle and visceral pain by their causes and symptoms. Muscle pain often stems from acute episodes, while visceral pain involves nerve and emotional impact. Healthcare providers face diagnostic challenges, requiring management strategies, lifestyle modifications, and treatment options.
What Is the Best Example of Visceral Pain?
You’ll find appendicitis is a prime example due to its common causes and severe symptoms. Diagnosis involves imaging, and treatment often requires surgery. Chronic conditions like IBD impact daily life, need management and support resources for relief.
What Is the Difference Between Parietal and Visceral Pain?
You’ll notice parietal sensitivity as sharp and localized, while visceral organs cause diffuse pain perception. Nociceptive signals from visceral nociceptors travel sensory pathways, often creating referred pain. Effective pain management requires understanding neural transmission and appropriate pain response.
Conclusion
In understanding visceral pain, recognizing its complex nature and how it differs from somatic pain is crucial. You should pay attention to the symptoms and characteristics, as they can guide accurate diagnosis. Knowing the causes helps you consider the best treatment options, including alternative therapies. Stay informed about current research trends to explore new approaches and enhance your management strategies. By doing so, you’ll improve your ability to address visceral pain effectively and compassionately.

