You’re probably familiar with the annoyance of heel pain, but have you ever considered it Achilles Tendinopathy Insertional? This condition’s not just about discomfort—it’s about understanding a complex interplay of factors like repetitive stress and biomechanical quirks. Imagine you’re an athlete or just someone who enjoys an active lifestyle; the last thing you want is a nagging pain that limits your range of motion. Spoiler alert: there are various treatment paths, but they require careful consideration. What if there was a way to get back on your feet without resorting to invasive measures?
Key Takeaways
- Insertional Achilles tendinopathy involves pain and swelling at the heel where the tendon meets the bone.
- Risk factors include repetitive stress, older age, diabetes, and poor footwear.
- Diagnosis typically involves a physical examination and imaging tests like X-rays or MRI.
- Non-surgical treatments include NSAIDs, physical therapy, heel lifts, and shock wave therapy.
- Surgical options may involve debridement and tendon transfer and can require lengthy recovery.
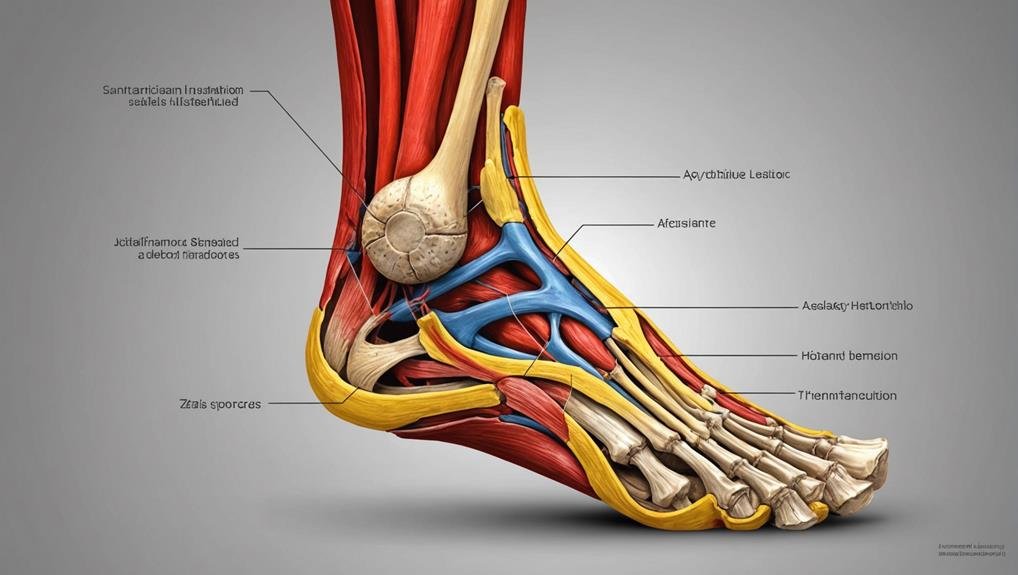
Understanding Achilles Insertional Tendinopathy
Achilles insertional tendinopathy is a condition that causes chronic damage and inflammation where the Achilles tendon meets the heel bone. If you’re dealing with this issue, it’s important to understand the risk factors involved. Repetitive stress from activities like running, older age, diabetes, and biomechanical problems such as foot pronation can all contribute to the development of this condition. Recognizing these factors can help you prevent or manage the situation.
A healthcare professional will perform a physical examination, review your clinical history, and order imaging tests like X-rays or MRI to confirm a diagnosis of Achilles insertional tendinopathy. These steps help pinpoint the exact nature of the heel’s damage and inflammation.
Regarding treatment options, conservative measures are usually the first approach. These might include rest, physical therapy, and modifications to your activities to reduce stress on the tendon. Surgical interventions may be considered if conservative measures don’t bring relief, especially in severe cases. Surgery aims to address the persistent issues and provide long-term relief. Understanding these aspects will empower you to make informed decisions about your condition and seek appropriate care.
Symptoms of Insertional Tendinopathy
You might notice a gradual onset of pain and swelling at the back of your heel, a hallmark of insertional Achilles tendinopathy. Jumping, running, or walking uphill can worsen this pain, making simple tasks uncomfortable.
This condition often causes tenderness and pain when you touch the affected area.
Gradual Heel Pain Onset
Experiencing a gradual onset of heel pain can be a telltale sign of insertional Achilles tendinopathy. This condition often creeps up on you, manifesting as a persistent, dull ache at the back of your heel. Initially, you might brush it off, but the symptoms become more noticeable as the pain continues.
You might feel tenderness and swelling around the heel, especially after engaging in certain activities. These symptoms are linked to the inflammation of the Achilles tendon at its insertion point.
Here are three key aspects of gradual heel pain onset in insertional Achilles tendinopathy:
- Pain and Swelling: The pain begins gradually and can be accompanied by noticeable swelling around the heel, making it difficult to wear certain shoes comfortably. This swelling can aggravate the pain and be irritating.
- Tenderness: You may notice tenderness when touching the affected area. This sensitivity is often most pronounced after periods of rest or inactivity.
- Activity-related Discomfort: While some activities can worsen the pain, it is crucial to recognize that even everyday movements can trigger discomfort in your heel. If overlooked, this can lead to further complications.
Activity-Induced Pain Worsening
Many find that activity-induced pain worsening is a vital characteristic of insertional Achilles tendinopathy. If you’re dealing with this condition, you might notice your pain intensifying during or after activities like running, jumping, or walking uphill. This exacerbation is often accompanied by a gradual onset of pain and swelling at the back of the heel, making daily activities more challenging.
Due to the swelling in the heel area, you might also experience painful rubbing in your shoes. This discomfort can turn simple tasks, like putting on shoes, into distressing ordeals.
Additionally, painful tendon stretching is another symptom you might encounter. This can limit your range of motion and make it difficult to perform exercises or stretches.
Tenderness upon touching the affected area is common in insertional tendinopathy. Even the lightest touch can cause discomfort, adding to the challenge of managing this condition. Recognizing these symptoms early is essential for effective treatment. By understanding that activity-induced pain worsening is a significant sign of insertional Achilles tendinopathy, you can take proactive steps to address it, potentially reducing the impact on your daily life and preventing further damage.
Causes and Risk Factors

Insertional Achilles tendinopathy often arises from repetitive stress and micro-trauma at the point where the Achilles tendon attaches to the heel bone, known as the calcaneus. This condition is influenced by several risk factors that you should be aware of.
As you age, the likelihood of developing insertional Achilles tendinopathy increases. Being overweight puts extra strain on your heel bone, aggravating the tendon. Additionally, if you have diabetes, your risk of experiencing this issue is heightened due to its effects on tissue health.
You might encounter extrinsic factors, such as sudden changes in your physical activity. For instance, if you suddenly decide to ramp up your exercise routine or change your workout habits, you could place undue stress on your tendon. Poor footwear choices and smoking also contribute to the problem. Recognizing these elements can help you manage your risk.
Here’s a quick list of factors to watch out for:
- Medications: Using fluoroquinolones or steroids can elevate your risk.
- Biomechanical Issues: Conditions like planus or forefoot hyperpronation can be contributors.
- Metabolic/Rheumatologic Diseases: These conditions increase your risk significantly.
Stay mindful of these to help prevent tendinopathy.
Diagnosis Techniques
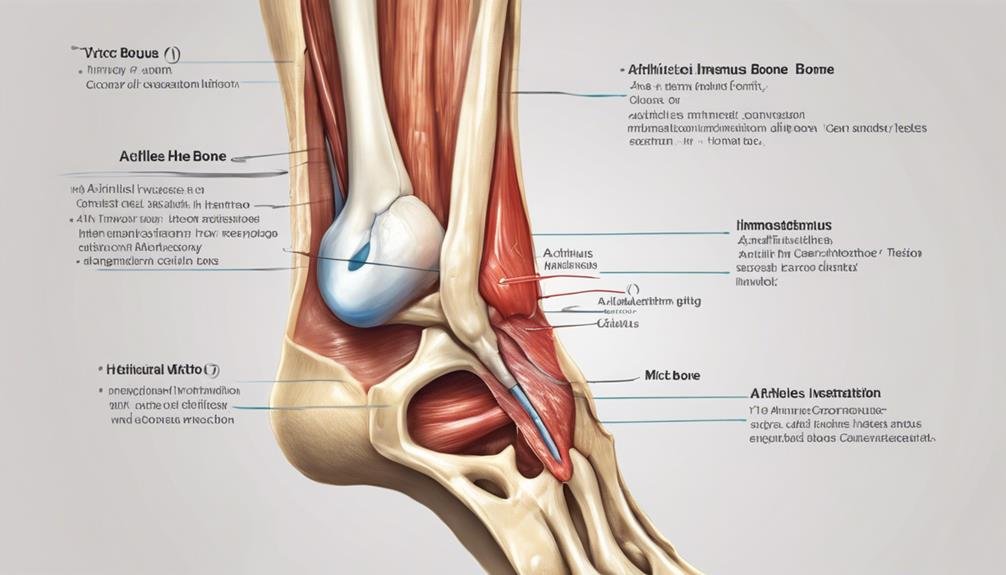
Diagnosing insertional Achilles tendinopathy typically starts with a thorough clinical examination by a foot and ankle orthopedic surgeon. During this exam, they’ll assess your symptoms and may perform specific tests to pinpoint the source of your discomfort. Most diagnoses involve imaging techniques to get a clearer picture of what’s happening inside your foot.
X-rays are pivotal in identifying structural changes, such as heel spurs or calcium deposits, often accompanying insertional Achilles tendinopathy. These images can reveal the presence of a heel spur, an outgrowth of bone that can irritate the surrounding tissues and exacerbate symptoms. While X-rays provide valuable insights into bone-related issues, they don’t show soft tissue like tendons.
MRIs might be employed for a more detailed view of the tendon itself. Although not always necessary for diagnosis, MRIs can help assess the severity of tendon damage, revealing issues that aren’t visible on X-rays. This inclusive approach guarantees that the diagnosis of insertional Achilles tendinopathy is accurate, paving the way for effective treatment strategies tailored to your specific condition.
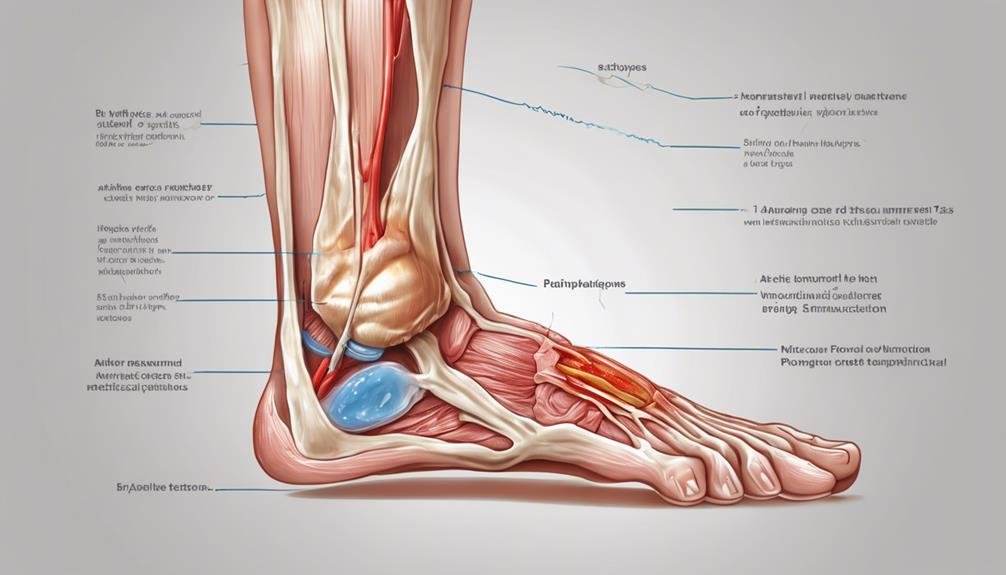
Non-Surgical Treatment Options

When dealing with insertional Achilles tendinopathy, non-surgical treatment options are often the first step towards relief. You can start by considering NSAIDs to help manage pain and inflammation. It’s essential to alleviate pressure on your tendon, so heel lifts and proper footwear can make a significant difference. These strategies reduce pain and swelling, making daily activities more comfortable.
Physical therapy plays a pivotal role in your recovery. Specific exercises like eccentric strengthening can help strengthen your affected tendon and improve function. These exercises are designed to stretch and load the tendon in a controlled manner, promoting healing over time.
In addition to the above, here are three more non-surgical treatments you might find beneficial:
- Night Splints: These can keep your heel flexed, reducing morning stiffness.
- Shock Wave Therapy: This treatment stimulates healing by delivering sound waves to the affected area.
- Temporary Braces can offer additional support and stability, addressing walking difficulties.
Surgical Treatment and Recovery
When non-surgical treatments don’t ease your symptoms, surgical options like removing diseased tendon sections or bone spurs might be necessary.
After surgery, expect a recovery period where you’ll likely wear a splint or cast boot, and full healing can take 9 months or more.
Be aware of potential complications, including ongoing pain, infections, or tendon avulsion.
Surgical Procedure Options
Understanding the complexities of surgical treatment for insertional Achilles tendinopathy involves comprehending the various options available. The primary goal is to relieve pain and restore function to the tendon.
Here are three common surgical procedures you might consider:
- Debridement: This surgical procedure targets removing diseased portions of the tendon and any bone spurs that may be irritating. By clearing these problem areas, debridement aims to reduce pain and improve tendon function.
- Gastrocnemius Recession: A gastrocnemius recession might be recommended if tension on the Achilles tendon insertion contributes to your condition. This procedure releases the stress on the tendon, potentially providing significant relief and aiding recovery.
- Tendon Transfer: A tendon transfer may be necessary in more severe cases of insertional Achilles tendinopathy. This involves relocating another tendon to support the damaged Achilles tendon, helping restore function and alleviate pain.
Recovery from these surgical options often requires wearing a splint or cast boot to protect your healing tendon. Keep in mind that full recovery can take nine months or longer, and there’s always a risk of continued pain post-surgery. It’s important to weigh these factors when considering surgery.
Post-Surgery Recovery Timeline
Setting off on the road to recovery after surgery for insertional Achilles tendinopathy requires patience and diligence. Your post-surgery recovery can take nine months or longer, so following the recommended recovery timeline is essential for the best outcomes.
Initially, you’ll likely need to wear a splint or cast boot to protect your healing tendon. This will allow it to mend properly without unnecessary strain.
Physical therapy plays a crucial role in your recovery, helping you regain strength and flexibility in your Achilles tendon. Engaging in targeted exercises will improve your mobility and support the healing timeline, but follow your therapist’s guidance closely to avoid setbacks.
Monitoring for potential complications is important. Be vigilant for signs of continued pain or wound infections, as these issues can hinder your progress. Promptly addressing any concerns with your healthcare provider will ensure you stay on track.
Stay committed to the process throughout your recovery timeline and communicate openly with your medical team. By adhering to the prescribed plan and being proactive about any complications, you’ll maximize your chances for a successful recovery and return to your daily activities stronger than ever.
Potential Surgical Complications
Managing recovery from surgical treatment for insertional Achilles tendinopathy involves being aware of potential complications. While surgery can provide relief, preparing for and recognizing any issues that might develop is vital. Knowing these possible surgical challenges can help you make informed decisions and take necessary precautions.
- Post-operative tendon avulsion or rupture is a serious risk where the tendon detaches after surgery. It can significantly prolong recovery and may necessitate additional interventions.
- Wound infections: Infections can occur at the surgical site, complicating recovery. Proper wound care and monitoring for signs of infection, such as redness or swelling, are crucial.
- Nerve damage and blood vessel injury: These are risks associated with surgical procedures. Damage to nerves can lead to numbness or tingling, while blood vessel injury may affect circulation and healing.
You might also experience continued pain or discomfort following surgery. This could be due to the initial condition persisting or new issues arising. Being proactive in your recovery, following your surgeon’s advice, and attending follow-up appointments can help mitigate these challenges, ensuring a smoother recovery path.
Potential Risks and Complications
Understanding the potential risks and complications is key when considering surgical intervention for insertional Achilles tendinopathy. Surgery might seem like a definitive solution, but it comes with its own set of challenges. Risks include infection, nerve damage, and continued pain, which can greatly impact recovery. These issues mightn’t only prolong your healing process and affect your overall mobility. Infection can lead to further procedures, while nerve damage may cause numbness or tingling. Continued pain is a reminder that surgery isn’t always a cure-all.
Complications don’t stop at the operating table. YouAfter-surgery, yought face delayed wound healing, tendon avulsion, or even tendon rupture pohese problems can hinder your return to normal activities and prolong rehabilitation. Long-term, you could experience stiffness, weakness, and a limited range of motion in your ankle. There’s also a risk of reoccurrence or persistent symptoms, meaning even after successful surgery, the issue mightn’t fully resolve.
Careful post-operative management is essential to minimize these risks. Following your healthcare provider’s instructions diligently ensures the best recovery and helps mitigate complications. Knowing these potential outcomes prepares you for a more informed decision-making process.
Prevention and Maintenance Strategies
Strong prevention and maintenance strategies are the foundation for preventing insertional Achilles tendinopathy. To protect your tendons, focus on regularly stretching and strengthening your calf muscles. This practice not only enhances flexibility but also builds resilience against strain. Pay attention to your footwear as well. Choosing shoes with good heel support can make a big difference in preventing discomfort and injury.
Consider these important steps:
- Progress Gradually: Avoid sudden spikes in exercise intensity. Gradually increase your activity levels to allow your body to adapt. Rest days aren’t just a luxury—they’re essential for tendon recovery and health.
- Address Biomechanical Issues: Regularly check for any biomechanical issues or foot abnormalities. Getting these assessed and corrected can prevent undue stress on your Achilles tendon.
- Maintain a Healthy Weight: Controlling your body weight reduces the load on your tendons. This proactive measure can go a long way toward preventing tendinopathy.
These strategies can help you maintain tendon health and keep you active without pain. Stay mindful of your body’s signals and adjust your routines to stay on track.
Conclusion
You’ve learned that Achilles Insertional Tendinopathy involves pain at the heel’s back, often due to repetitive stress and biomechanical issues. Diagnosis typically includes a physical exam and imaging tests. Effective treatment can range from NSAIDs and physical therapy to surgical options like debridement. Remember, post-surgery recovery demands patience and a strict adherence to a rehab plan. To prevent future issues, focus on proper footwear, stretching, and strengthening exercises to maintain tendon health.
FAQs
What is insertional Achilles tendinopathy?
Insertional Achilles tendinopathy is where the lower portion of the Achilles tendon, near its insertion at the heel bone, becomes inflamed and painful. This often results from repetitive strain, overuse, or sudden increases in physical activity. Insertional tendinopathy can cause stiffness, pain, and swelling at the back of the heel.
Key Points:
- Inflammation at the heel bone insertion
- Caused by repetitive strain or overuse
- Symptoms: pain, swelling, stiffness at the back of the heel
What are common symptoms of insertional Achilles tendinopathy?
Symptoms typically include pain at the back of the heel, especially during activities like walking or running, and stiffness, particularly in the morning. Swelling and tenderness around the heel are also common. Over time, the condition may worsen without proper treatment, making it difficult to perform regular activities.
Key Points:
- Pain and stiffness at the heel, especially in the morning
- Swelling and tenderness at the Achilles tendon insertion
- Symptoms worsen with activity and over time
How is insertional Achilles tendinopathy treated?
Treatment includes rest, ice, and nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation. Physical therapy with specific exercises, like heel lifts and eccentric strengthening, can help improve flexibility and strength. Severe cases may require shockwave therapy or, in rare cases, surgical intervention.
Key Points:
- Rest, ice, and NSAIDs for immediate relief
- Physical therapy for strength and flexibility
- Advanced treatments: shockwave therapy or surgery if needed